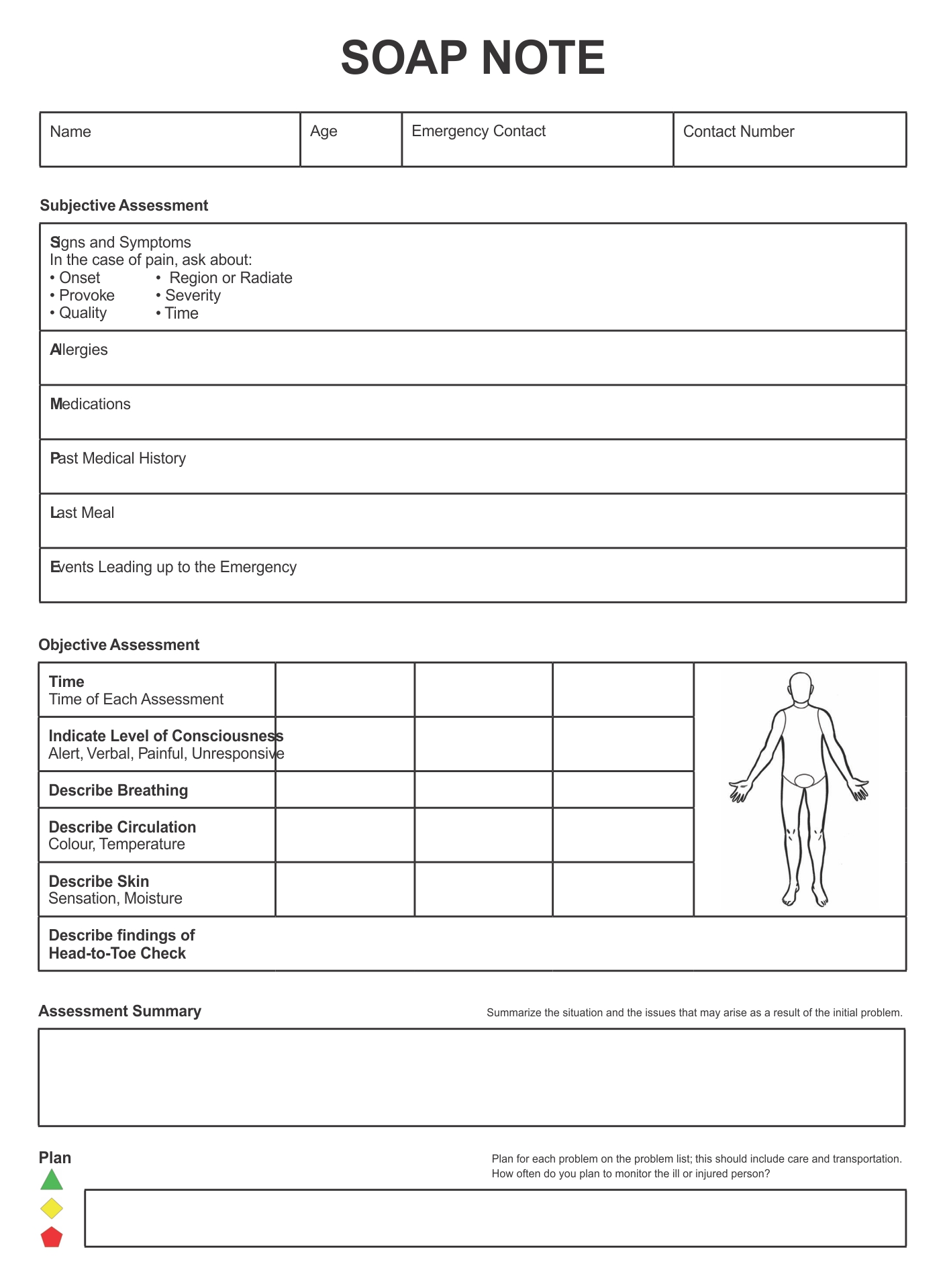
When you see a chiropractor, they may fill out a SOAP note in addition to the usual medical forms. It will look similar to a medical form, but with some key differences. A SOAP note should have a table of content and a row for the patient’s complaint, complete with checkboxes for severity. The patient’s name, date of checkup, and complaint type should all be provided. Printable Chiropractic Forms SOAP Note
What Are Chiropractic SOAP Notes?
A chiropractor’s SOAP notes are a way to document patient information and support accurate billing and coding. During a patient visit, the chiropractor should note the patient’s chief complaint and any findings that relate to the patient’s condition. Often, the patient’s first-hand account of the problem and any findings from the physical examination should be included.
Often, a chiropractor will also use SOAP notes as a way to streamline the flow of a patient visit. The SOAP format helps chiropractors structure their patient visits and help patients feel heard. In addition, this format is helpful when submitting claims, since it allows doctors to capture important patient information more quickly.
SOAP notes are a universal and consistent way for chiropractors to document the care provided to a patient. They also ensure that chiropractors follow all healthcare guidelines and get paid by insurance companies. The SOAP note software offered by health can help doctors create SOAP notes in just a few easy steps.
How Do You Fill Out A SOAP Note For A Chiropractor?
The SOAP note is an important document for chiropractors. It records interactions with patients and the progress of treatments to improve the quality of care. It is also a vital piece of documentation that ensures payment for services. A SOAP note includes the patient’s firsthand description of the problem and the results of a physical examination.
A chiropractor’s SOAP note should include important information about the patient’s diagnosis and treatment plan. It should also note the patient’s response to the treatment and their rehabilitation goals. It is important to follow the proper format when writing these notes. There are several tips to make sure that your notes are legible and accurate.
SOAP notes are an essential part of the healthcare industry. These notes are a valuable tool for tracking the progress of a patient and ensuring compliance with HIPAA regulations. A chiropractor must keep SOAP notes for every single patient visit. These notes should be comprehensive, easy to read, and compliant. To help chiropractors achieve this, the industry’s leading EHR software packages include SOAP note functionality.
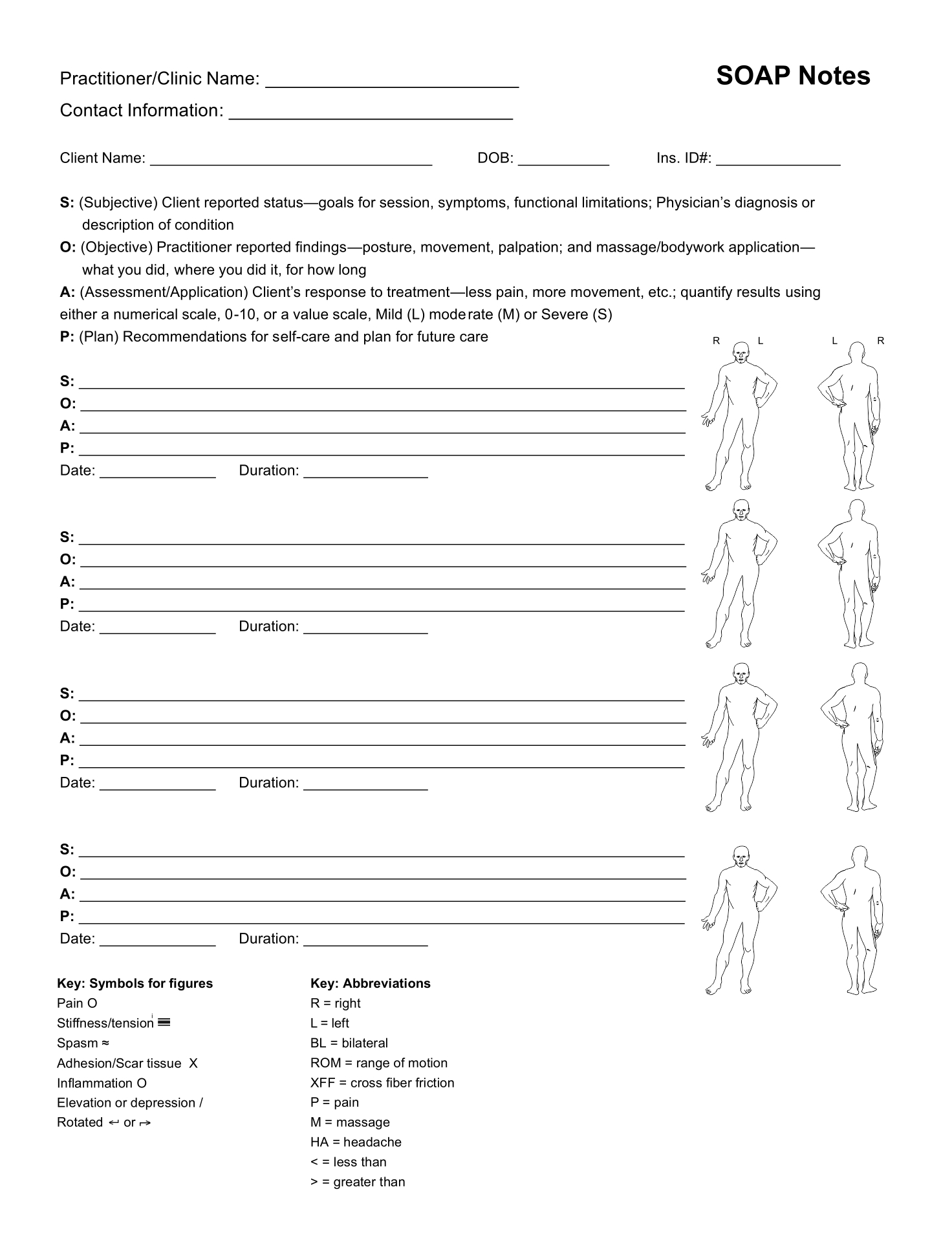
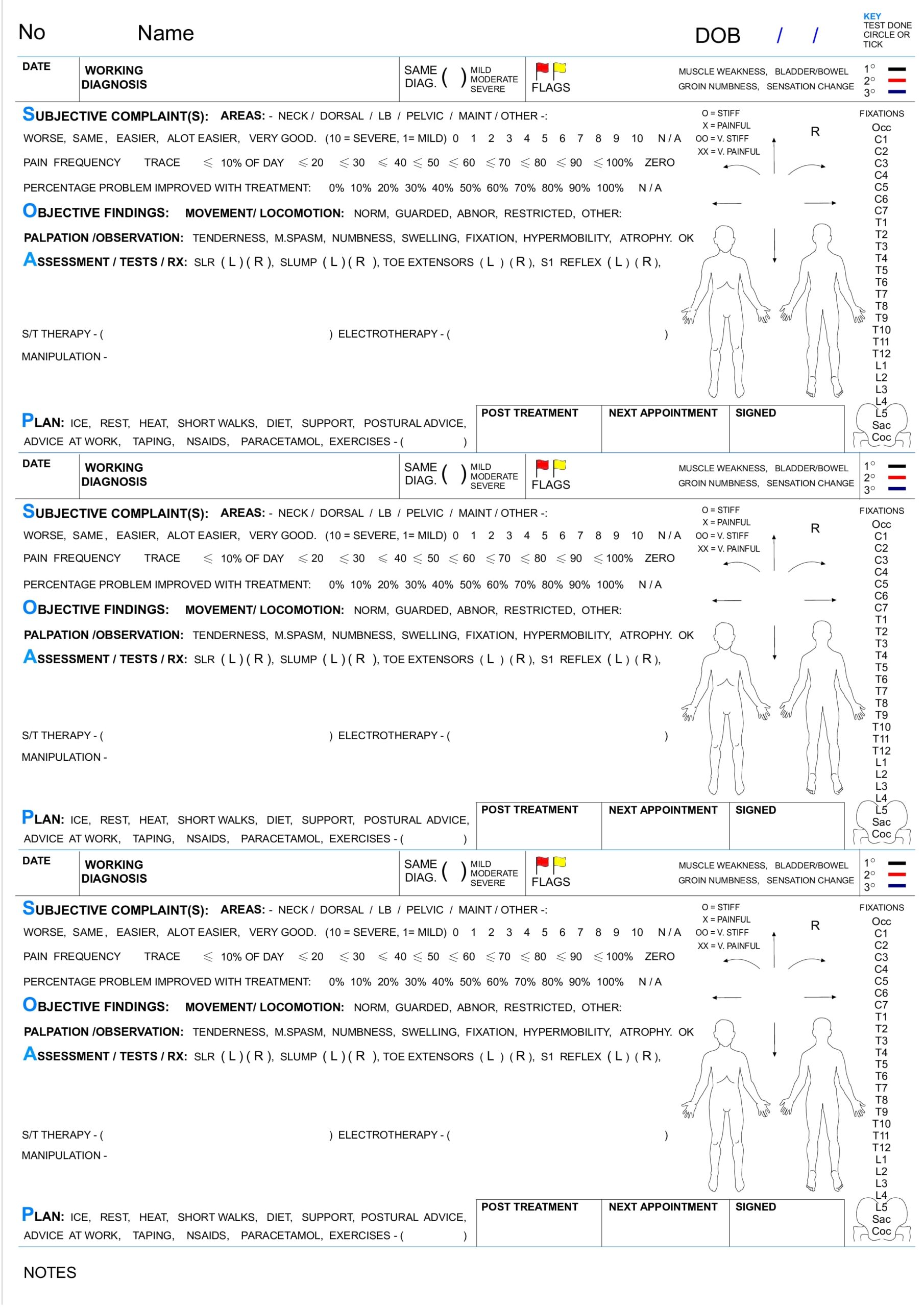
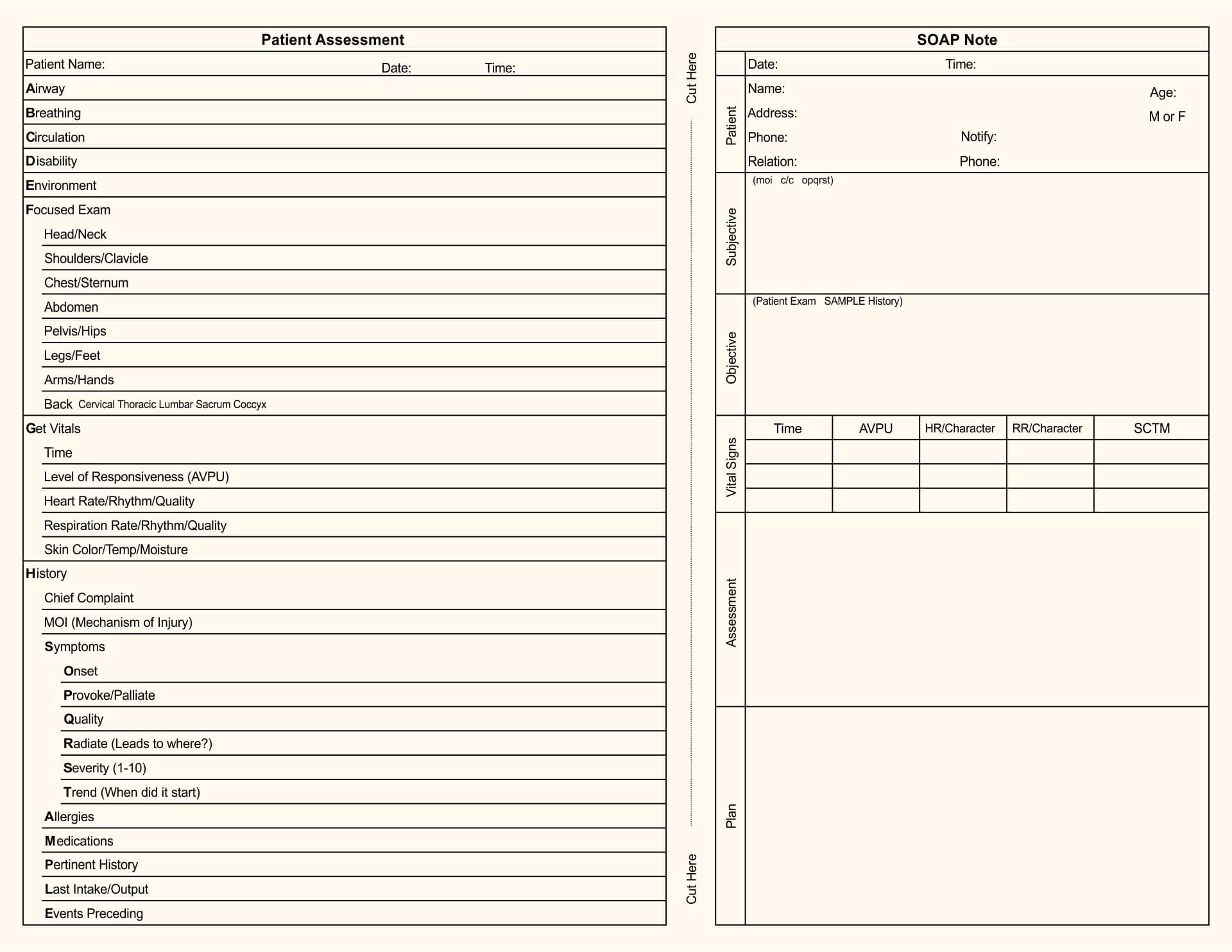
Printable Chiropractic Forms SOAP Note
If you are a chiropractor, you should be familiar with how to fill out a SOAP note. This form is used for collecting information about a patient, as well as writing down checklists. SOAP stands for Subjective, Objective, Assessment, and Plan, and chiropractors must follow the guidelines that are set forth in this form. Fortunately, there are several forms you can find online that can help you with this task.
A SOAP note is used to document the adjustments that were performed during a patient visit. It also includes information about the treatments provided. The SOAP note should contain all relevant information, including the diagnosis, treatment plan, and patient assessment. It also should include daily notes that help establish medical necessity and justify continued care.
A SOAP note is an essential part of any chiropractic practice. It will help you keep track of important notes from patient visits and will ensure compliance with HIPAA regulations. It will also help you get paid by insurance companies.