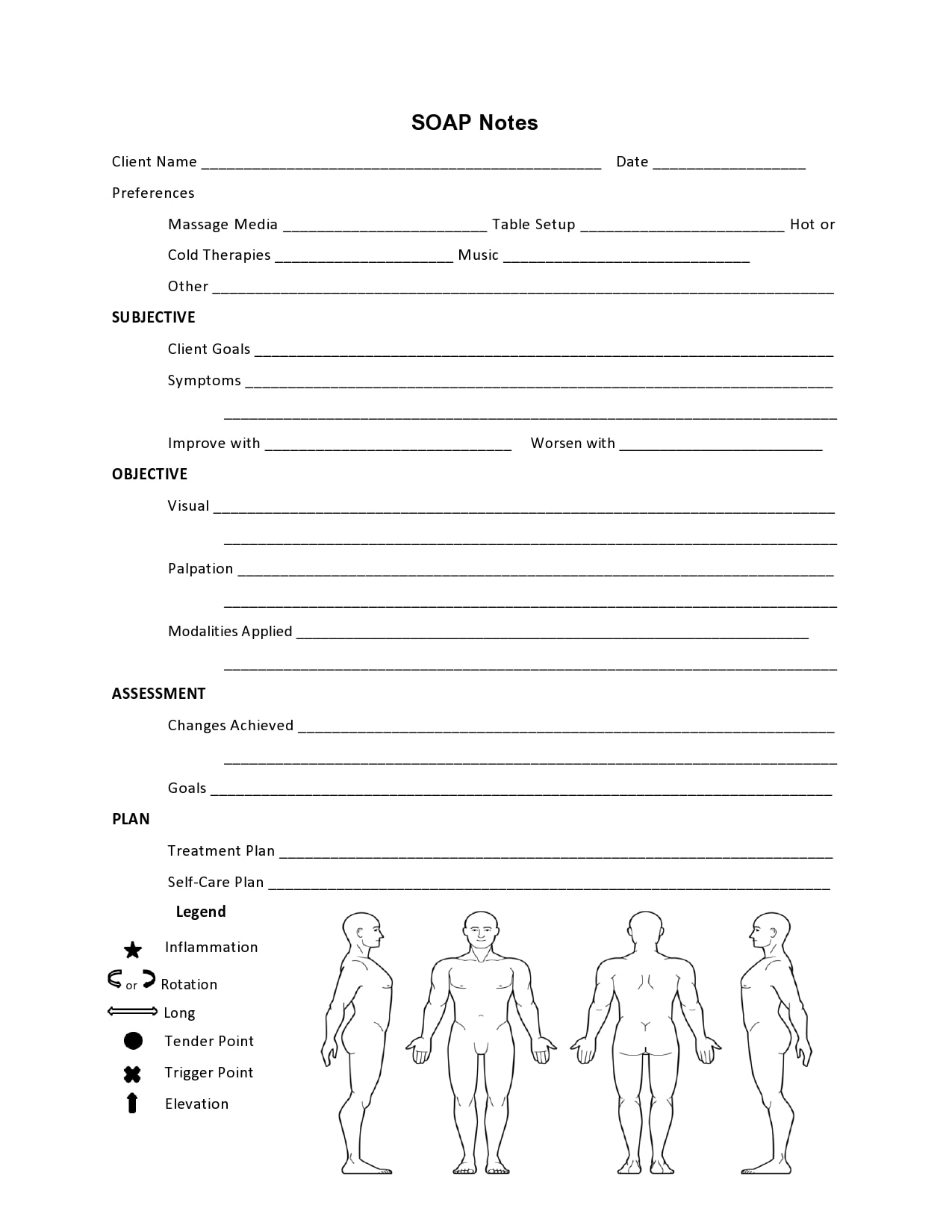
In this article, we’ll cover the purpose of SOAP notes and how to write them. SOAP notes are intended to organize and manage a treatment plan. You can use a SOAP note template to help you keep track of the details of a client’s treatment. This tool can help you organize your notes and manage your caseload more effectively.
How To Write A Counseling SOAP Note?
A SOAP note is a useful document for tracking client progress and making adjustments to treatment plans. It should not contain unsourced opinions or statements. Instead, it should contain specific data relating to the client’s current mental state and treatment plan. Furthermore, it should avoid vague verbs and content that is repetitive or unclear.
SOAP notes are written after a session. It is important to take notes after every appointment. They should be written in a neutral tone and should include quotations from the session. In addition, they should be recorded in an Electronic Health Record platform. SOAP notes can save a lot of time and effort. High-quality notes can contribute to improved health outcomes.
First, start by identifying the chief complaint. This can be a symptom or a physical condition. In addition, it can be an experience that has the patient in an unhappy mood. Identifying the chief complaint is essential for a thorough diagnosis.
What Is The Purpose Of A SOAP Note Template?
The SOAP note template is a document that includes information on the mental status of the client. It includes objective information, such as appearance and speech, as well as subjective information, such as mood and effects. It should also document the patient’s progress. The information provided should be documented and analyzed in order to make adjustments in the treatment plan as needed. SOAP notes can be written in different ways, but chronological order is most effective.
Typically, a SOAP note will be one to two pages long, with most sections being 1-2 paragraphs long. This format allows the notes to provide a detailed description of the session without becoming overly complex. The information contained in SOAP notes is also easily shared among providers within the same group.
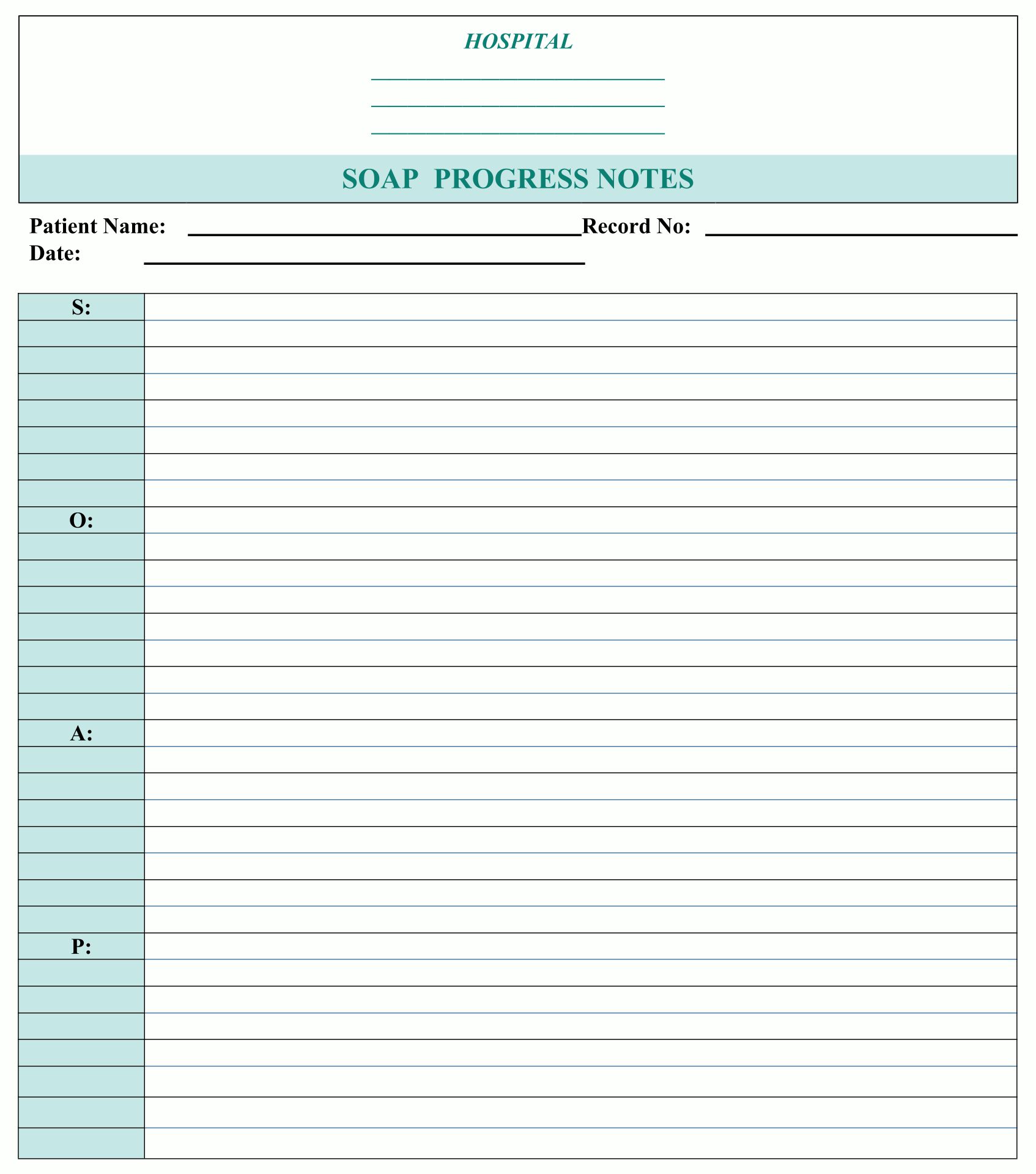
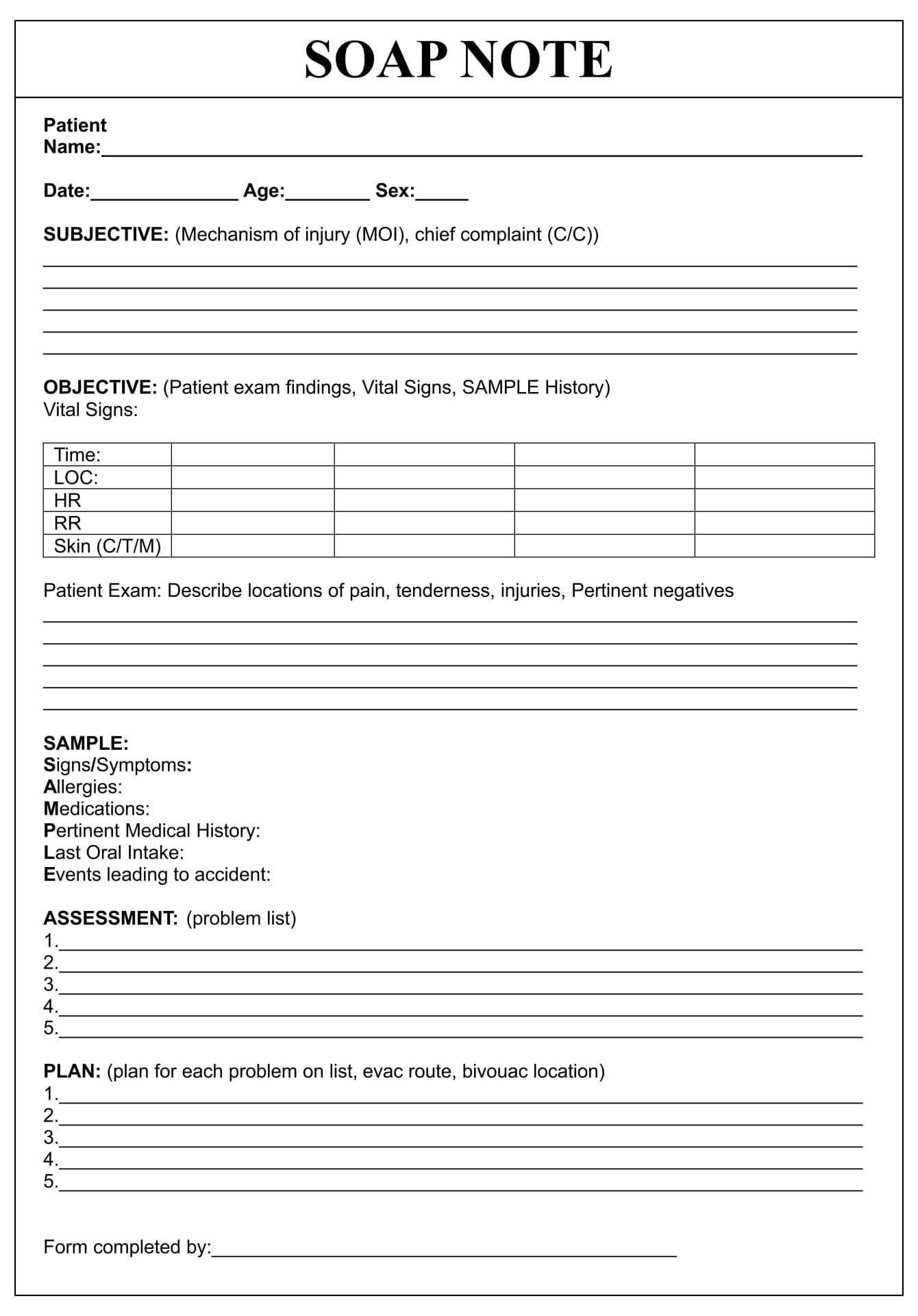
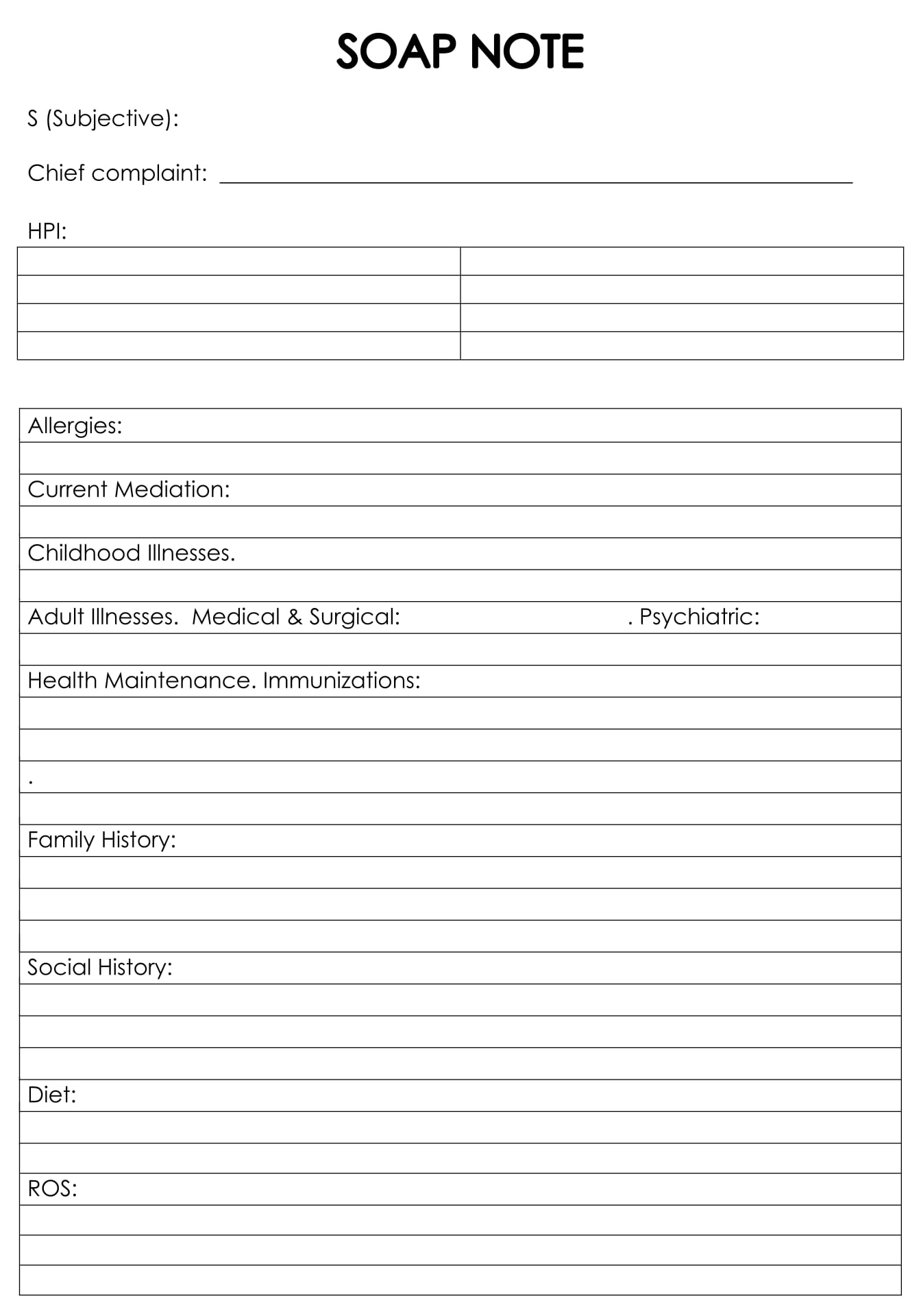
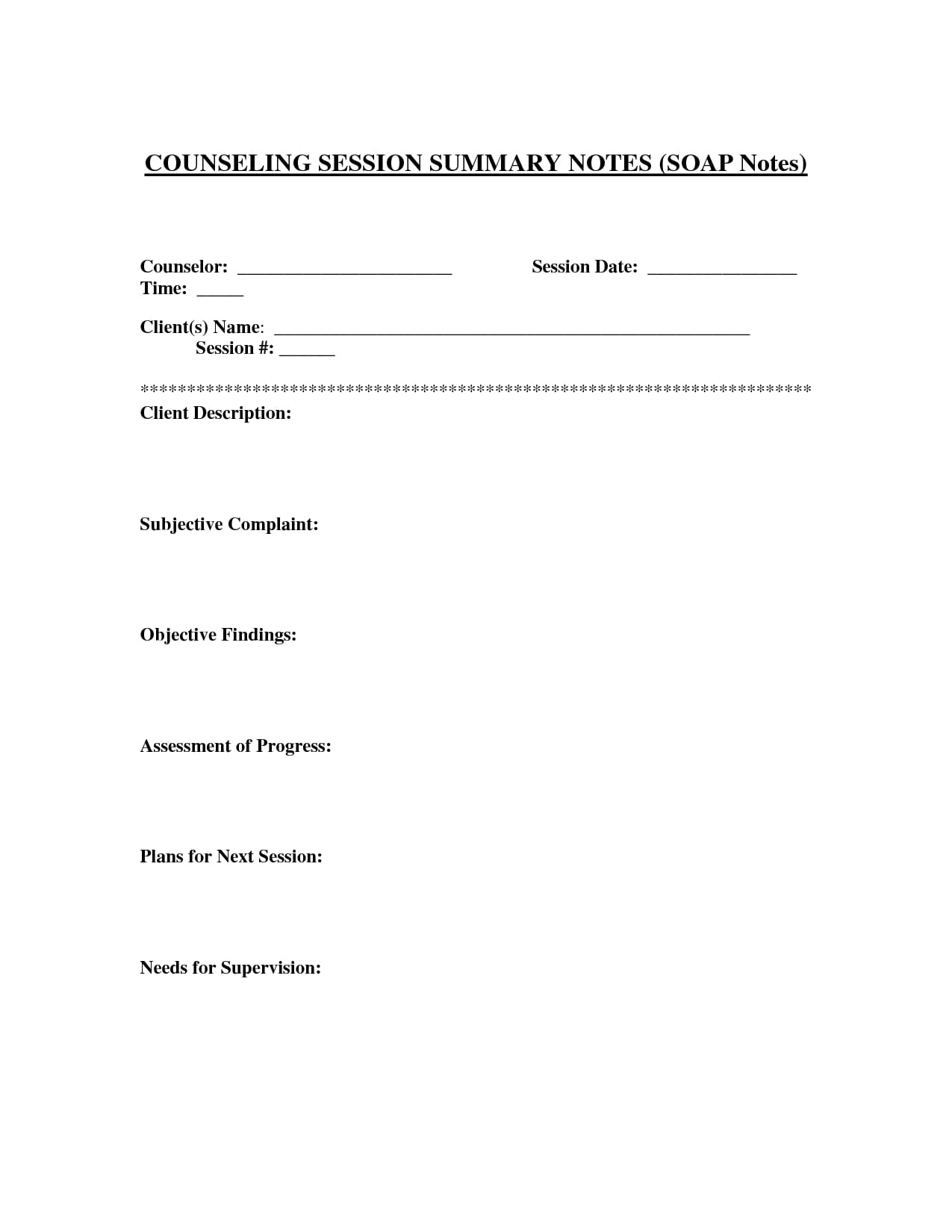
Printable Counseling SOAP Note Templates
A SOAP note is a form that is often used in counseling sessions. It outlines the current treatment plan and any changes that have occurred in the client during the course of the session. The notes should be short, detailed, and organized in a standard format. The notes should also be re-ordered with the assessment and plan at the top, making it easier to find specific information.
SOAP notes are a key component of streamlined healthcare, and they can play a major role. Although they are not as sophisticated as e-prescribing or robust mental health features, they are an essential component for many practitioners. By providing consistent and clear information about each patient’s progress, SOAP notes help better equip counselors and therapists.
SOAP notes have been around for several decades, and they remain popular because they’re so effective. They were developed in the 1960s by Dr. Lawrence Weed as a way for physicians to document patient histories and make better clinical decisions. They have improved the health of millions of patients worldwide. Printable Counseling SOAP Note Templates